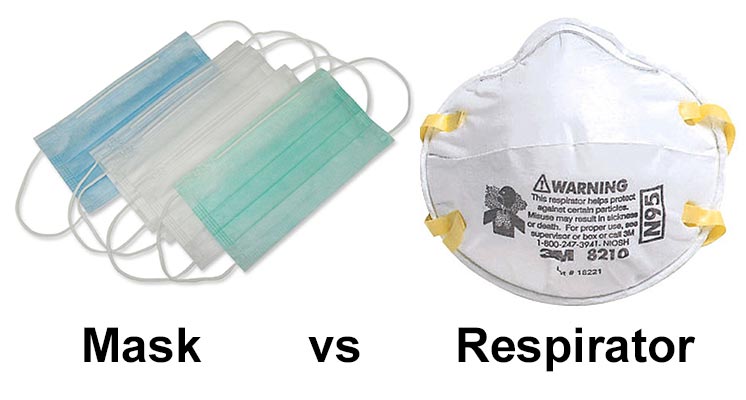
Masks vs Respirators
Before we go any further, let’s just clarify on a technical difference between a “mask” and a “respirator”. In day to day language we often say mask, when referring to what are technically called respirators.
Uses for Masks:
- Masks are loose fitting, covering the nose and mouth
- Designed for one way protection, to capture bodily fluid leaving the wearer
- Example – worn during surgery to prevent coughing, sneezing, etc on the vulnerable patient
- Contrary to belief, masks are NOT designed to protect the wearer
- The vast majority of masks do not have a safety rating assigned to them (e.g. NIOSH or EN)
Uses for Respirators:
- Respirators are tight fitting masks, designed to create a facial seal
- Non-valved respirators provide good two way protection, by filtering both inflow and outflow of air
- These are designed protect the wearer (when worn properly), up to the safety rating of the mask
- Available as disposable, half face or full face

Respirator Standards
Whilst surgical style masks are not redundant by any means (discussed more below), they aren’t designed to protect the wearer, whilst respirators are.
The US Center for Disease Control (CDC) cites the N95 respirator standard as part of the advised protective equipment in their Covid-19 FAQ and their SARS guidance (SARS being a similar type of Corona virus). Which suggests that an N95 or better respirator is acceptable.
N95 vs FFP3 & FFP2
The most commonly discussed respirator type is N95. This is an American standard managed by NIOSH – part of the Center for Disease Control (CDC).
Europe uses two different standards. The “filtering face piece” score (FFP) comes from EN standard 149:2001. Then EN 143 standard covers P1/P2/P3 ratings. Both standards are maintained by CEN (European Committee for Standardization).
Let’s see how all the different standards compare:
| Respirator Standard | Filter Capacity (removes x% of of all particles that are 0.3 microns in diameter or larger) |
|---|---|
| FFP1 & P1 | At least 80% |
| FFP2 & P2 | At least 94% |
| N95 | At least 95% |
| N99 & FFP3 | At least 99% |
| P3 | At least 99.95% |
| N100 | At least 99.97% |
As you can see, the closest European equivalent to N95 are FFP2 / P2 rated respirators, which are rated at 94%, compared to the 95% of N95.
Similarly, the closest to N100 are P3 rated respirators – with FFP3 following closely behind.
You could approximate things to say:

Actual data source from 3M official website As you see above, N95 and FFP2 are not different.
As you see above, N95 and FFP2 are not different.
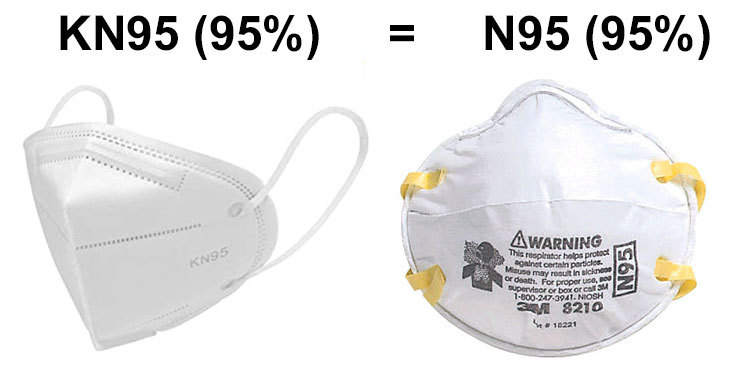
KN95 vs N95
According to 3M (source), the Chinese KN95 standard has an equivalent specification to N95/FFP2 respirators . To quote:
“It is reasonable to consider China KN95, AS/NZ P2, Korea 1st Class, and Japan DS FFRs as equivalent to US NIOSH N95 and European FFP2 respirators”
In practice the issue is more complex, and I wouldn’t take for granted that all KN95 respirators are up to the same standard.
Things to watch out for:
- Typically KN95 respirators are held in place by over-ear elastic loops, rather than behind the head elastics. This can result in a weaker seal. Fortunately there are methods for tightening – see this YouTube video for ideas. Products called “ear savers” can also aid with tightening, and can be found on eBay or you can 3D print them.
- There’s no guarantee that all KN95 respirators actually meet the Chinese KN95 standard. However, with the current respirator shortage, unfortunately the same goes for N95/FFP also.
The KN95 specification is referred to as GB 2626-2006 (preview here) – so you will generally see that written on the KN95 respirators. From July 1st 2020, it’ll be replaced by GB 2626-2019, an updated specification (preview here).
I’ve linked below to a supplier of KN95 respirators in the USA – in case it’s of use to some readers.
Valve vs Non-Valved Respirators

Valved respirators make it easier to exhale air. This makes them more comfortable to wear, and leads to less moisture build-up inside the respirator. Ideal for things like DIY/construction work.
The problem with valved respirators is that they do not filter the wearer’s exhalation, only the inhale. This one-way protection puts others around the wearer at risk, in a situation like Covid-19. It’s for this reason that hospitals and other medical practices do not use valved respirators.
One hack to protect (and respect) others when wearing a valved respirator is to put a surgical mask or “cloth face covering” over the valved respirator, to (partially) filter the out breath.
TL;DR – yes, respirators with high efficiency at 0.3 micron particle size (N95/FFP2 or better) can in theory filter particles down to the size of the coronavirus (which is around 0.1 microns). What that doesn’t tell us is how much protection respirators will provide against coronavirus when in use – we will need to wait for future studies to confirm.
Read on to learn more…
A recent paper shows that the coronavirus ranges from between 0.06 and 0.14 microns in size. Note that the paper refers to the coronavirus particle as 2019-nCoV, which was it’s old name. The virus is currently called SARS-CoV-2, and the illness it presents in people is called Covid-19.

Respirator’s are measured by their efficiency at filtering particles of 0.3 microns and bigger (noting that the coronavirus is smaller than that).
The reason for the focus on 0.3 microns is because it is the “most penetrating particle size” (MPPS). Particles above this size move in ways we might anticipate, and will get trapped in a filter with gaps smaller than the particle size. Particles smaller than 0.3 microns exhibit what’s called brownian motion – which makes them easier to filter. Brownian motion refers to a phenomenon whereby the particle’s mass is small enough that it no longer travels unimpeded through the air. Instead it interacts with the molecules in the air (nitrogen, oxygen, etc), causing it to pinball between them, moving in an erratic pattern.
According to researchers this point between “normal” motion and brownian motion is the hardest particle size for filters to capture.
What we can take away from this, is that high filter efficiency at 0.3 micron size will generally translate to high filter efficiency below this size also.
For more discussion and details on the subject of respirator filters and brownian motion – see this great post at smartfilters.com.

Now lets look at specific research that measures the filter efficiency at 0.3 microns and below (coronavirus territory)…
- This article by 3M discusses research showing that all 6 of the N95 respirators they tested can efficiently filter lower than 0.1 micron size with approximately 94% efficiency or higher. The graph below is from that article, and illustrates this:
- Additionally, smartfilters.com have a great article on this subject, citing research showing that the respirators tested could filter down to 0.007 microns (much smaller than Covid-19). For example the 3M 8812 respirator (FFP1 rated) was able to filter 96.6% of particles 0.007 microns or larger. Suggesting FFP2 or FFP3 would achieve even greater filtration.
The below image (click it to expand) shows the size of the coronavirus, relative to other small molecules like a red blood cell, or the often talked about PM2.5 particle size.

Image of coronavirus vs other particles – from smartairfilters.com
Reliable Brands?
Prior to the pandemic, there was easy access to reliable brands such as 3M, GVS, Moldex etc. Now, however, their supply is either going to frontline workers, or, it’s quite limited.
This means that the general public are left to either make their own face coverings (discussed below), or do their own due diligence when sourcing less well known brands. Hopefully the above content helps with that due diligence process.
Below I’ve listed a US retailer who currently have stock, ship to mainland USA, and I’ve bought from personally with no issues:
Health Bodyguard Store
KN95 rated respirators from Health Bodyguard Store, stocked in Ohio, from $4 per respirator. See my brief review of their KN95 respirators for more info.
Surgical Masks
Surgical masks are generally speaking a 3-ply (three layer) design, with 2 sheets of “non-woven” fabric sandwiching a “melt-blown” layer in the middle. It’s the melt-blown layer that provides the filtering capability. A melt-blown material is also used in respirators, and thus you can imagine it’s more expensive and hard to come by recently, due to demand.

Image of the melt-blown filaments under microscope come from mdpi.com
The melt-blown fabric is made by melting a plastic, then blowing it from either side at high velocity onto a rotating barrel. Done right, this results in a fabric composed of tiny filaments. For a more technical (!) explanation of the process – see here.

Diagram of melt-blown machinery (left) comes from Erdem Ramazan’s book, and the image of melt-blowing in progress (right) comes from 4FFF on wikipedia
Not all melt blown fabric has the same filtering capability, some are better than others. Unfortunately we can’t test the filtering capability of the melt-blown layer without specialized knowledge and equipment. What we can do, however, is at least check that the melt-blown layer is present.
Below I show an example of a surgical mask (left) that came without the melt-blown layer. You can imagine that, given the extra cost and current scarcity of melt-blown fabrics, manufacturers might cut corners with this layer, so it’s worth keeping an eye on.
Choosing surgical masks that have been tested according to a set of standardized test methods (ASTM F2100, EN 14683, or equivalent) will help avoid low quality products. The ASTM standard for surgical masks (particularly levels 2 & 3) are primarily focused around fluid resistance during surgery. These higher levels don’t offer much extra in the way of protection from Covid-19 under non-surgical conditions.

Whilst FFP2/FFP3 or N95/N100 are the gold standard as far as face protection goes, what about surgical masks, do they provide any protection?
Strictly speaking, surgical masks are primarily designed to protect vulnerable patients from medical professionals. Stopping the wearer (e.g. surgeon) from spreading their germs when coughing/sneezing/speaking. So they’re designed to protect patients, not to protect the wearer.
An obvious flaw with surgical masks compared to respirators is their lack of a tight face fit, which leaves gaps around the edges.
There isn’t currently research available on the efficacy of surgical masks (or even respirators), for protecting wearers against the coronavirus. Although this isn’t totally surprising given how new the virus is.
In lieu of that, the below looks at research around the use of surgical masks and N95 masks in the context of influenza, looking specifically at the protection given to the wearers. Influenza may be a good virus particle to compare it to, as they are both transmissible through droplets and aerosol, both cause respiratory infection, and both are similar in particle size.
N.B. Please don’t conflate the comparison to the influenza particle as suggestion that they are comparable illnesses – current data suggests that the coronavirus may have a higher mortality rate.

Source for coronavirus (SARS-CoV-2) size is this paper, whilst sources for Influenza size are this paper (eventually published in Vaccine), and a Frontiers in Microbiology paper.
In the first study we will look at, 2,862 US health care personnel were split into 2 groups, those wearing N95 masks and those wearing surgical masks1. There were 207 lab confirmed influenza events in the respirator wearing group, compared to 193 in the mask wearing group – a difference that was not statistically significant.
In the next study, Canadian nurses were split into 2 groups, those wearing N95 masks and those wearing surgical masks. There were 50 cases of influenza in the surgical mask group, compared to 48 in the N95 respirator group2. Again, no significant difference.
So where does this leave us? Those 2 studies suggest that surgical masks are approximately comparable to N95 masks when it comes to preventing influenza illness in close contact clinical settings. What this doesn’t tell us, is whether they’re better than wearing nothing on our faces.
To find that out, we need a study that has a control group that doesn’t use any facial protection. Due to ethical considerations, those studies aren’t abundant, but we do have at least one.
In this Australian study, they looked at 286 adults in 143 households who had children with influenza-like illness3. For clarity, influenza-like illness is not the same as laboratory confirmed influenza. It’s diagnosed by symptoms like fever, dry cough and feeling sick, which could mean influenza, but could also be caused by the common cold or other viruses. They found that adults who wore masks in the home were 4 times less likely than non-wearers to be infected by children in the household with a respiratory infection. There is nice analysis of the study here by Imperial College London.

Image via smartairfilters.com
It’s definitely fair to note that this Australian study was very small, and could not be considered definitive by any means. That being said, we’ve got to work with what he have, and this at least gives us some data points:
- Wearing a surgical mask or N95 (FFP2) respirator was better (in the study) at protecting against influenza-like illnesses than wearing nothing at all
- Whilst we can anticipate surgical masks to be inferior to respirators, the studies above suggest they are not as inferior as one might assume. For example the first two studies didn’t find a significant difference between surgical masks and N95 respirators, when protecting wearers against influenza.
- Important to note that we’ve used influenza protection as a proxy for SARS-CoV-2 (coronavirus). This is done because SARS-CoV-2 is new and there are no comparable studies on it. But of course the drawback is that it still leaves a lot of uncertainty, as SARS-CoV-2 may act quite differently in terms of transmission.
In a lab setting, with artificial conditions, we find that surgical masks are able to block 80% of particles down to 0.007 microns. Compared to the 3M 8812 respirator in this study which blocked 96% (FFP1 rated). This generally aligns with our discussion above.

Image via smartairfilters.com
In conclusion: we don’t know how much protection surgical masks provide against the novel coronavirus. However, the above at least suggests that a surgical mask may provide more than zero protection – and that’s worth being aware of. It makes sense to only wear them for protection as a method of last resort – with respirators being the primary choice.
It is much safer to avoid the company of people who are sick or potentially sick, and to reduce social contact overall, especially to large groups of people (see the social distancing section below). To repeat, the use or surgical masks would have to be a last resort – and wearing one should not encourage anyone to take unnecessary exposure risks.
If we are in the presence of someone sick, who has/might have the coronavirus, it makes sense for them to wear a mask or respirator to reduce their ability to spread the disease.
Article by fastlifehack blog (https://fastlifehacks.com/n95-vs-ffp/)















